Diabetes Mellitus and Metabolic Syndrome—When Your Pancreas Develops Trust Issues.
The Plot Twist Your Body Didn't See Coming
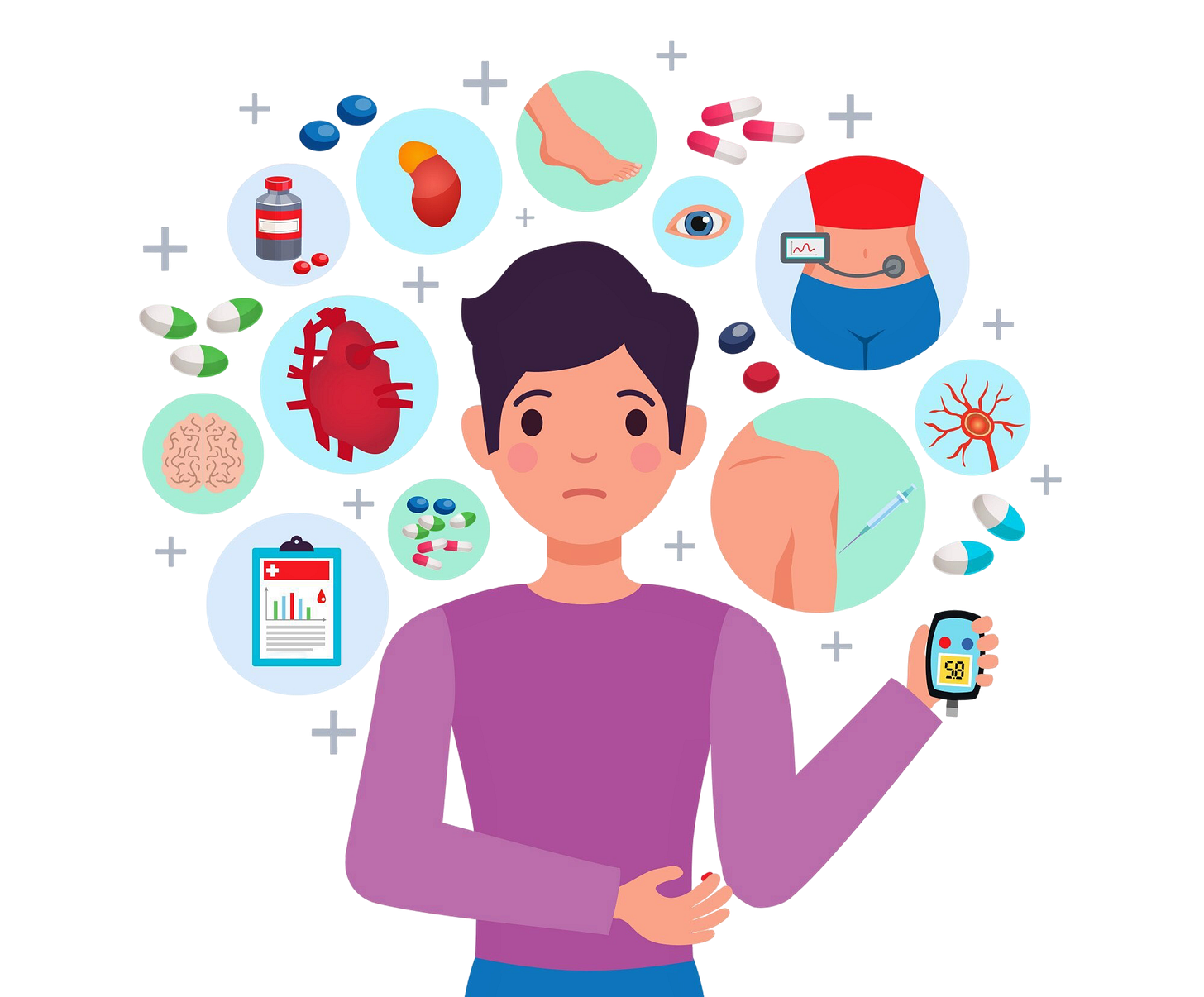
Imagine your body as a finely tuned orchestra, with every metabolic process playing in perfect harmony. Now picture two disruptive forces—diabetes mellitus and metabolic syndrome—barging in like off-key musicians, turning that beautiful symphony into chaos. Unfortunately, this isn't fiction. With 463 million adults globally living with diabetes in 2019 and projections reaching 700 million by 2045, we're witnessing a metabolic pandemic that's rewriting the rules of human health.
Welcome to the first post of our diabetes and metabolic syndrome series at NutriNom, where we'll unravel this complex story and discover how these conditions became the uninvited guests at humanity's health party.
Diabetes Mellitus: When Blood Sugar Goes Rogue
Think of diabetes as your body's security system gone haywire. Normally, insulin acts like a master key, unlocking cells to let glucose enter and provide energy. In diabetes, this system breaks down, leaving glucose stranded in the bloodstream like party-goers locked out of the venue.
Type 1 Diabetes (10% of cases): The autoimmune rebel where the body's immune system mistakenly destroys insulin-producing cells. It typically appears in childhood, though it can strike at any age. While genetics load the gun, environmental triggers—possibly viral infections—pull the trigger.
Type 2 Diabetes (90% of cases): The lifestyle-influenced troublemaker characterized by insulin resistance. Cells become stubborn, refusing to respond to insulin's signals. This type has a complex inheritance pattern—having one parent with Type 2 diabetes increases your risk by 15-25%, but lifestyle factors often determine whether those genetic cards get played.
Gestational Diabetes: The temporary visitor during pregnancy that usually leaves after delivery but warns of future Type 2 diabetes risk.
Metabolic Syndrome: The Perfect Storm
If diabetes is a single storm, metabolic syndrome is a weather system brewing multiple storms simultaneously. It's diagnosed when you have central obesity (waist circumference >102 cm for men, >88 cm for women) plus any two of these troublemakers:
High triglycerides (≥150 mg/dL)
Low "good" HDL cholesterol
High blood pressure (≥130/80 mmHg)
Elevated fasting glucose (≥100 mg/dL)
Research shows that 42% of diabetic patients also have metabolic syndrome, making this a dangerous double act.
The Toxic Relationship: How They Feed Each Other
Here's where our story gets sinister. Metabolic syndrome and diabetes don't just coexist—they actively make each other worse through a vicious cycle:
Act 1: The Setup: Excess weight, particularly around the midsection, triggers inflammation and insulin resistance. Fat cells, especially visceral fat, release inflammatory substances that interfere with insulin's ability to do its job.
Act 2: The Struggle: Your pancreas tries to compensate by producing more insulin. For a while, this works—blood sugar stays normal despite the resistance. But this is like shouting louder when someone won't listen; eventually, you'll lose your voice.
Act 3: The Breaking Point: The pancreas becomes exhausted and can't produce enough insulin to overcome the resistance. Blood sugar rises, progressing from normal → pre-diabetes → Type 2 diabetes. People with metabolic syndrome are 5 times more likely to develop diabetes than those without it.
Reading the Warning Signs
Diabetes symptoms often follow a predictable pattern:
Frequent urination and excessive thirst (your kidneys working overtime)
Unexplained weight loss despite normal appetite
Persistent fatigue (cells starving despite high blood sugar)
Blurred vision and slow-healing wounds
Metabolic syndrome is trickier—it's often silent except for an expanding waistline. This stealth factor makes it particularly dangerous.
Catching the Culprits: Diagnosis
Diabetes diagnosis requires any one of:
Fasting glucose ≥126 mg/dL
HbA1c ≥6.5% (your 2-3 month glucose average)
Glucose tolerance test ≥200 mg/dL
Metabolic syndrome diagnosis needs that central obesity plus two additional criteria mentioned earlier.
The Treatment
The good news? Both conditions respond dramatically to lifestyle changes. Think of it as editing your body's story rather than accepting the current plot.
The Food Chapter:
Focus on complex carbohydrates, lean proteins, and healthy fats
Aim for 10-15g daily fiber intake
Practice portion control (smaller plates work wonders)
Limit sodium to 6g daily
The Movement Chapter:
Minimum 30 minutes of exercise, 5 days weekly
Mix cardio with resistance training
Start small—even taking stairs counts
The Sleep & Stress Chapter:
Prioritize 7-9 hours of quality sleep
Manage stress through proven techniques
Poor sleep and chronic stress directly worsen insulin resistance
Rewriting the Ending: Prevention and Reversal
For Everyone: The Universal Prevention Plan
Maintain a healthy weight (BMI <25)
Stay physically active
Choose nutrient-dense foods
Avoid tobacco and limit alcohol
Monitor your numbers regularly
For the High-Risk: Emergency Action Plan
If you're on the edge of diabetes or already have metabolic syndrome, here's your roadmap to recovery:
The 7% Solution: Studies show that losing just 7% of body weight can reduce Type 2 diabetes risk by 58%.
Daily Game-Changers:
Replace one sugary drink with water
Add a 10-minute walk after meals
Fill half your plate with vegetables
Practice mindful eating—slow down and savor
Set a consistent sleep schedule
The Monitoring Strategy:
Check fasting glucose annually if low-risk, every 6 months if high-risk
Monitor blood pressure and lipid levels
Track waist circumference (the most telling measurement)
The Hopeful Plot Twist
Here's the beautiful part of this story: unlike many genetic conditions, diabetes and metabolic syndrome are largely preventable and often reversible. Your body has an remarkable ability to heal and adapt when given the right tools.
The Iraqi national guidelines emphasize that aggressive control of multiple risk factors simultaneously—not just blood sugar—provides the greatest protection. This isn't about perfection; it's about progress and giving your body the support it needs to rewrite its metabolic story.
Stay tuned and subscribe to NutriNom for more evidence-based nutrition and health knowledge! Our next blog post will continue our diabetes and metabolic syndrome series with "Insulin: The Unsung Hero—or the Rogue Agent?" We'll take a deep dive into insulin's fascinating dual nature, uncover the mechanisms behind insulin resistance, and explore exactly what goes wrong at the cellular level when diabetes and metabolic syndrome take hold.
Remember: every day you make choices that either support or sabotage your metabolic health. The power to influence this story's ending is literally in your hands—and on your plate.