The FTO Gene: Your Molecular Nemesis in the War Against Adiposity
The Gene That Makes You Hungry—Forever
Weight Loss Management Series - Finale
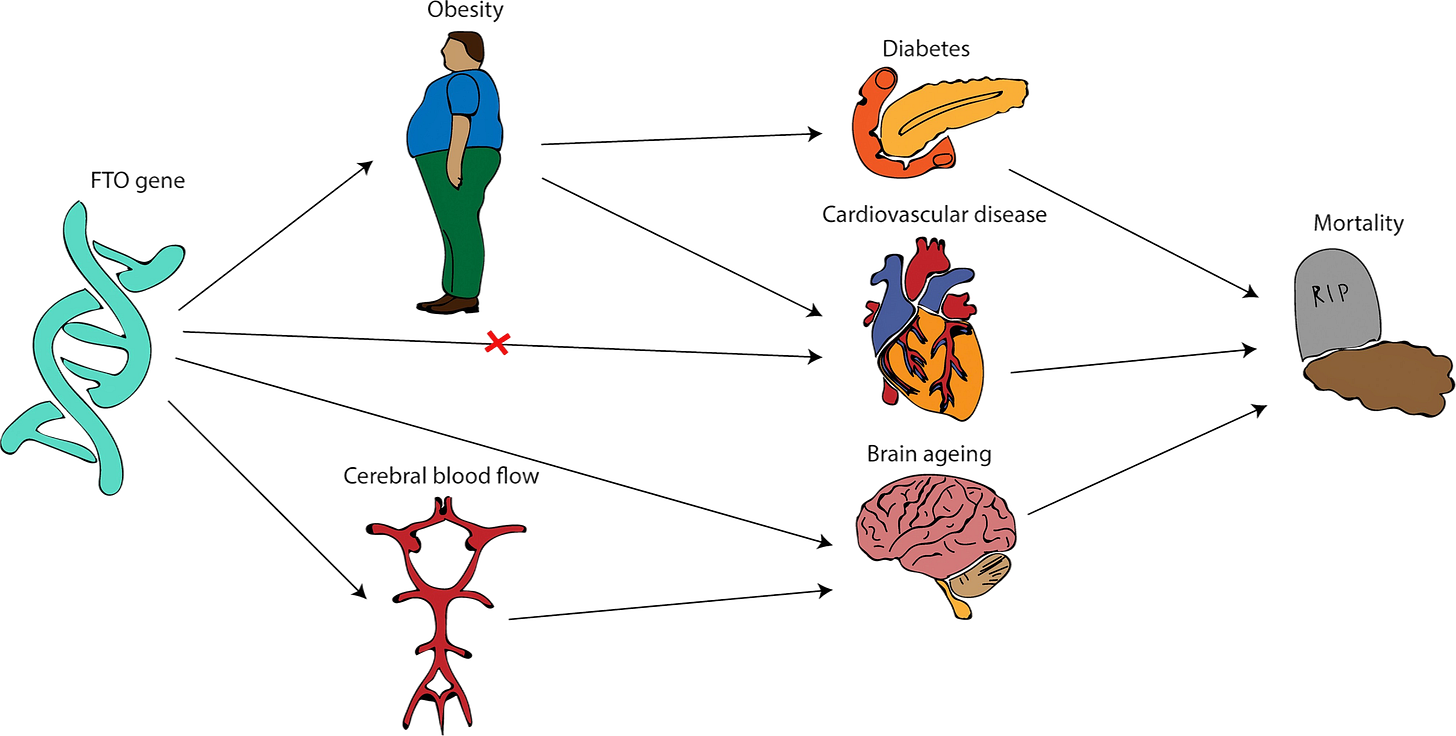
Welcome to the culmination of our Weight Loss Management series, where we examine the genetic puppeteer that has been orchestrating your nocturnal refrigerator raids since the dawn of civilization. Today's protagonist: the notorious FTO gene, or as I like to call it, "The Fat Troublemaker Orchestrator."
The Historical Context: When Survival Met Surplus
Let us briefly revisit the Pleistocene epoch, when our ancestors faced the formidable challenge of intermittent food availability. Natural selection, in its algorithmic wisdom, favored individuals possessing enhanced energy storage capabilities. Enter the FTO gene—initially humanity's survival insurance policy, now operating more like an overenthusiastic accounts receivable department that never learned to stop collecting.
The irony is almost poetic: the same genetic adaptation that once ensured survival through famine now manifests as the leading genetic factor in modern obesity pathogenesis. It's rather like discovering your insurance policy includes unlimited coverage for events that no longer occur.
Molecular Mechanisms: The Biochemical Farce
The Ghrelin Symphony in A-Minor (Emphasis on Minor)
The FTO protein functions as an N6-methyladenosine demethylase, preferentially targeting ghrelin mRNA transcripts. For our colleagues requiring translation from biochemistry-speak: imagine ghrelin as a text message from your stomach reading "Food please," and the FTO risk allele as that friend who forwards every message five times with increasing urgency.
The molecular cascade proceeds thusly:
FTO demethylates ghrelin mRNA
Ghrelin expression increases (approximately 40% in risk carriers)
Hypothalamic appetite circuits activate with operatic intensity
Patient experiences what they describe as "constant hunger" (what neuroscientists term "persistent orexigenic signaling")
Neuroimaging Evidence: When fMRI Screenshots Reveal the Unthinkable
Functional magnetic resonance imaging studies have captured the neural drama in exquisite detail. Risk allele carriers demonstrate:
Pre-prandial state: Enhanced activation in the medial orbitofrontal cortex (translating "calorie-dense food" into "immediate priority")
Post-prandial state: Persistent ventral tegmental area activation (dopamine essentially asking "but is there dessert?")
Food-cue exposure: Hyperresponsivity in the amygdala and ventral striatum (emotional eating's command center throwing a parade)
In essence, their brains treat a photograph of a cheeseburger with the same reverence others reserve for their research h-index scores.
Global Epidemiology: The Genetic Geography Lesson
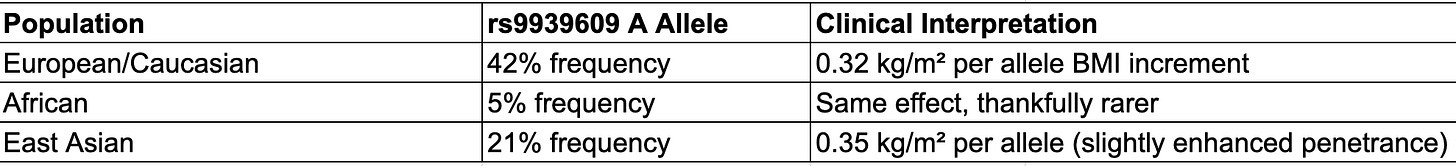
The mathematics are sobering: with additive inheritance patterns, homozygous carriers effectively begin life with a 3 kg handicap. It's rather like starting a marathon with ankle weights—theoretically manageable, but requiring acknowledgment and strategic compensation.
Clinical Manifestations: The FTO Pheno-Type
The Daily Struggle: A Case Study in Hedonic Regulation
Consider the quotidian experience of the AA genotype patient:
Standard Morning:
07:00: Balanced breakfast consumed
10:00: Mild hunger sensation
FTO-Enhanced Morning:
07:00: Breakfast completed
07:30: Niggling awareness of cafeteria donuts
08:00: Active resistance of snack vending machine
09:00: Lunch venue planning initiates
10:00: Snack resistance protocols failing
Food Preference Deviation Syndrome
Risk carriers demonstrate statistically significant preference patterns:
24% increased calorie-dense food selection
18% larger portion size requests
42% greater snacking frequency
Philosophical alignment with foods categorized as "appetizers," "desserts," and "that extra slice"
Essentially, their dietary choices suggest someone programmed their metabolic software with debug parameters permanently enabled.
The Therapeutic Paradox: When Disadvantage Becomes Treatment Response
Here's where our narrative takes an unexpected turn worthy of a peer-reviewed plot twist. Meta-analytical data (n=6,951 across 10 studies) reveals risk carriers achieve superior weight loss outcomes with structured interventions:
Additive Model Results:
AA vs TT: -0.44 kg (95% CI: -0.79, -0.09; p=0.015)
TA vs TT: -0.18 kg (95% CI: -0.45, 0.09; p=0.19)
The clinical interpretation? The same genetic variant that predisposes to obesity paradoxically enhances treatment responsiveness—evolution's version of a diagnostic apology note.
Evidence-Based Interventions: The Precision Nutrition Playbook
Genotype-Stratified Macronutrient Optimization
For AA Homozygotes (this represents having two copies of the "risk" allele associated with increased obesity susceptibility):
High-protein diet (25% of total energy intake)
Mechanism: Protein-induced satiety compensates for impaired endogenous signaling via GLP-1 and PYY upregulation
Low-fat protocol (≤20% energy) to minimize reward circuit activation
For AT Heterozygotes (these individuals have one copy of the risk allele (A) and one copy of the normal allele (T)):
Low-fat emphasis with moderate protein
Strategy capitalizes on partial phenotype expression
For TT Homozygotes (Two copies of the non-risk allele (normal)):
Standard dietary recommendations suffice
These fortunate souls may proceed with conventional nutrition algorithms
Lifestyle Modification Protocols
Fiber Supplementation Strategy
Minimum 30g daily soluble fiber
Acts as caloric absorption inhibitor (think "nutritional adblocker")
Promotes short-chain fatty acid production for appetite regulation
Chrononutritional Intervention
Time-restricted feeding windows (12-14 hours)
Capitalizes on circadian lipid oxidation patterns
Essentially hacking the body's overnight fat-burning subroutines
Environmental Restructuring
Remove visual food cues from clinical and home environments
Implement portion control through pre-portioned options
Consider it preventive maintenance for willpower
Physical Activity Prescription
Moderate exercise reduces genetic risk by 67%
Even 150 minutes weekly substantially attenuates phenotype
Think of it as installing a metabolic system update
Clinical Success Metrics: Real-World Applications
Institutional Case Studies:
Patient Gamma (AA genotype, endocrinology department):
Baseline: BMI 32, constant prandial dissatisfaction
Intervention: High-protein protocol + chrononutrition
Outcome: 16% body mass reduction, reported "actual appetite satisfaction—novel concept"
Patient Delta (TA genotype, bariatric clinic):
Protocol: Standard low-fat diet optimization
Result: 12% mass reduction, maintenance at 18-month follow-up
The Meta-Analysis That Changed Everything
Recent systematic reviews have fundamentally altered our understanding of FTO-mediated obesity. Risk carriers don't just respond to treatment—they respond with statistical enthusiasm that borders on the remarkable:
Enhanced weight loss response (SMD: -0.619)
Improved metabolic parameter normalization
Sustained adherence rates exceeding baseline population
The implications are profound: genetic predisposition to obesity may paradoxically predict enhanced treatment response, suggesting a biological compensation mechanism worthy of further investigation.
Clinical Conclusions: Reframing Genetic Determinism
Dear colleagues, the FTO gene represents not a metabolic death sentence, but rather an opportunity for precision medicine application. While 42% of your patients may be genetically predisposed to enhanced appetite signaling, they are equally predisposed to enhanced treatment response.
Consider this genetic variant as less of a diagnostic limitation and more of a therapeutic opportunity. After all, if evolution handed us a metabolism that hoards energy like a post-apocalyptic survivalist, science has handed us the countermeasures to navigate our current post-scarcity environment.
Tune in for our next academic adventure: "Diabetes Mellitus and Metabolic Syndrome—When Your Pancreas Develops Trust Issues." Because after mastering genetic weight regulation, surely endocrine dysfunction will seem like child's play...
If this genomic exposition has provided clinical value whilst maintaining academic standards, consider supporting our mission to translate research into accessible practice. Because the gap between laboratory and clinic room should be bridged with evidence, not rhetoric.
Subscribe to our professional channels for continued evidence-based content that neither condescends nor obfuscates.
P.S. The next time a patient attributes treatment failure to "genetics," you may now respond with 5,000+ citations worth of evidence suggesting their genes might actually be their secret weapon. Deploy this knowledge judiciously.